You are only seeing posts authors requested be public.
Register and Login to participate in discussions with colleagues.
Medical Journal News
Predatory Journals — What Can We Do to Protect Their Prey?
New England Journal of Medicine, Ahead of Print.
Categories: Medical Journal News
Bladder Stone
New England Journal of Medicine, Volume 392, Issue 2, January 9, 2025.
Categories: Medical Journal News
See the Harm
New England Journal of Medicine, Volume 392, Issue 2, Page 112-113, January 9, 2025.
Categories: Medical Journal News
Coordinating Multidisciplinary Care — Improving Outcomes after Fragility Fractures
New England Journal of Medicine, Volume 392, Issue 2, Page 109-111, January 9, 2025.
Categories: Medical Journal News
The Plight of “Dual Noneligible” People in the United States
New England Journal of Medicine, Volume 392, Issue 2, Page 105-107, January 9, 2025.
Categories: Medical Journal News
Texas Executive Order GA-46 and the Erosion of Trust in Health Care
New England Journal of Medicine, Volume 392, Issue 2, Page 107-109, January 9, 2025.
Categories: Medical Journal News
[Editorial] Can we turn the tide on NCDs in 2025?
In 2011, the UN Political Declaration on Non-Communicable Disease (NCD) Prevention and Control announced a target date of 2025 to reduce rates of premature mortality from cardiovascular diseases, cancers, chronic respiratory diseases, and diabetes by 25%—the so-called 25 × 25 goal. 10 years later, the global probability of prematurely dying from one of those targeted NCDs had improved by only 1·5%. NCDs are the leading causes of premature death and disability worldwide, estimated in 2021 to be responsible for the deaths of 17·3 million people and nearly 80% of all years lived with disability before the age of 70 years.
Categories: Medical Journal News
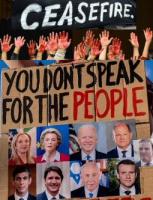
[Comment] Offline: Whispers from the Imperial Capital
The assassination of Brian Thompson, UnitedHealthcare's Chief Executive Officer, on Dec 4, 2024, in New York City, has catapulted American medicine, with all of its tragic inconsistencies and injustices, once again into the political spotlight. With the words “deny”, “depose”, and “defend” inscribed on three bullet casings, attention was drawn to the questionable practices of America's health insurance companies. They faced allegations of delaying payments, denying settlements, and defending obstructive behaviours by tying patients up in expensive litigation.
Categories: Medical Journal News
[Perspectives] Sabina Faiz Rashid: building social justice in public health
Professor Sabina Faiz Rashid is the Mushtaque Chowdhury Chair in Health and Poverty and the Director of the Center of Excellence for Gender, Sexual and Reproductive Health and Rights at the BRAC James P Grant School of Public Health, BRAC University in Dhaka, Bangladesh. She is also an Honorary Professor at the Liverpool School of Tropical Medicine in the UK. Through her 30-year career she has “continued to work on health and poverty and gender, and rights, expanding how public health is defined…critiquing how gender and health is understood, and how public health itself is very disease centric, despite evidence indicating that health is deeply interconnected to housing, food, jobs, water and sanitation, environment, and many other structural factors”, Rashid explains.
Categories: Medical Journal News
[Perspectives] A clinical certification pathway for generalist medical AI systems
There have been extensive evaluations of artificial intelligence (AI) systems for narrow medical tasks, but more work is needed to systematically evaluate and deploy AI systems that can perform a broad range of medical tasks. The medical training process itself might offer a template for addressing this challenge. Clinicians undergo rigorous education and training, progressing through stages of increasing responsibility and autonomy. Similarly, generalist medical AI systems could be subjected to a phased certification model before they are granted greater autonomy in patient care.
Categories: Medical Journal News
[Perspectives] Gabriel's gift
Tamarin Norwood is a member of a club nobody wants to join. It is not short of members. UNICEF records around 1·9 million stillbirths annually and 4·0 stillbirths per 1000 births occurred in the UK in 2023, rising to 6·3 for Black mothers. Other club members are people who miscarry (of which I am one), experience ectopic pregnancy, have a molar pregnancy, or have terminations for medical reasons. Prevalence of loss is higher in many low-income countries, and access to pregnancy and baby loss care varies depending on state and country legislation.
Categories: Medical Journal News
[Perspectives] Appetite for destruction
War and the Mind, a temporary exhibition at IWM London, UK, asks what it is within the human mind that initiates and maintains conflict, and how conflict, in turn, affects the workings of the human mind. Its focus is on wars in which the UK has engaged since the outbreak of World War 1 in 1914; however, it sets these in a wider context, with the first room featuring digital projections of neurons, brains, orchestras, and construction. Our brains are formed of cooperative networks, and this is reflected in the great joint endeavours that form human civilisation.
Categories: Medical Journal News
[Obituary] Frances Krauskopf Conley
Trailblazing neurosurgeon. She was born on Aug 12, 1940, in Palo Alto, CA, USA, and died on Aug 5, 2024, in Sea Ranch, CA, USA, of complications from dementia, aged 83 years.
Categories: Medical Journal News
[Correspondence] Salvage treatment of multi-refractory primary immune thrombocytopenia with CD19 CAR T cells
Primary immune thrombocytopenia is an autoimmune disease in which autoreactive B cells play a crucial role in pathogenesis by producing autoantibodies primarily directed against platelet surface glycoproteins (eg, glycoprotein IIb/IIIa; fibrinogen receptor) that trigger platelet destruction, resulting in severe thrombocytopenia. The annualised incidence of primary immune thrombocytopenia is approximately 3·3 cases per 100 000 people among adults.1 Despite several treatment options, including approved thrombopoietin receptor agonists and commonly used antibody-reducing approaches—such as B-cell depletion with the anti-CD20 monoclonal antibody rituximab, BTK inhibitors, SYK inhibitors, corticosteroids, and splenectomy—a subset of patients develop refractory immune thrombocytopenia.
Categories: Medical Journal News
[Correspondence] The legacy effect of hyperglycaemia in type 2 diabetes
Amanda I Adler and colleagues provided the striking evidence that the legacy effect of hyperglycaemia extends for up to 42 years of follow-up.1 Previous meta-analyses evidenced that the legacy effect becomes more apparent with a progressive longer duration of follow-up, but the benefit is not observed when only the events recorded during the observational phases of the trials are considered.2 The data presented by the authors might suggest a possible increasing benefit over time for intensive therapy, especially compared with the incidence of myocardial infarction.
Categories: Medical Journal News
[Correspondence] The legacy effect of hyperglycaemia in type 2 diabetes
We read Amanda I Adler and colleagues’ study on intensive glycaemic control in type 2 diabetes with keen interest. The 24-year post-trial follow-up provides unprecedented long-term insights.1 However, we have identified areas for enhancement.
Categories: Medical Journal News
[Correspondence] The legacy effect of hyperglycaemia in type 2 diabetes – Authors' reply
We thank Francesco Prattichizzo and Antonio Ceriello, and Ruirui Hou and Jian Ren for their interest in our Article.1 Examining UK Prospective Diabetes Study (UKPDS) observational data separately is difficult because adjusting appropriately for survivor effects is problematic. We continue to prefer to analyse the entirety of the data according to primary randomisation categories. The glycaemic legacy effect was seen with all randomised therapies used in the UKPDS, suggesting that the mode of glucose lowering is less important than achieving good glycaemic control.
Categories: Medical Journal News
[Correspondence] Decompressive craniectomy for people with intracerebral haemorrhage: the SWITCH trial
We read with great interest the SWITCH trial,1 which is an important amendment to the literature on the role of decompressive craniectomy for deep-seated intracranial haemorrhage. We applaud the authors for the trial. Sample size calculation was based on a dichotomised modified Rankin scale (mRS) 5–6 versus 0–4 and the primary analysis follows all recommendations in clinical trial planning, analysis, and reporting. However, the study's interpretation is overly optimistic and concerning. Death (mRS 6) has been exchanged by high-level dependence (mRS 4) among participants undergoing decompressive craniectomy and no secondary outcomes suggest benefit: the analysis dichotomised at mRS 0–3 versus 4–6 was neutral; quality of life measures at 180 years and 365 years were essentially the same; and permanent residential care at 180 days (71% vs 62%) and 1 year (43% vs 38%) was high in both groups and underpowered to detect a detrimental result.
Categories: Medical Journal News
[Correspondence] Decompressive craniectomy for people with intracerebral haemorrhage: the SWITCH trial
The SWITCH trial advances knowledge regarding the optimal management of large, deep intracerebral haemorrhage.1 This study showed a small benefit for decompressive hemicraniectomy in addition to optimal medical management for minimising death or severe disability (modified Rankin scale 5–6) at 6 months. A substantial proportion of the observed benefit was driven by reductions in mortality in the intervention group. However, the authors do not elaborate on the rates of withdrawal of life-sustaining therapy (WOLST) in each group, or if there was a protocolised approach to goals of care conversations.
Categories: Medical Journal News
[Correspondence] Decompressive craniectomy for people with intracerebral haemorrhage: the SWITCH trial
The SWITCH trial by Jürgen Beck and colleagues showed a trend towards improved 6-month outcome (although not statistically significant) when deep intracerebral haemorrhage was treated with decompressive craniectomy in addition to best medical treatment, and even had no effect if the modified Rankin score of 4 was considered a poor outcome.1
Categories: Medical Journal News